Even though I was born and raised in New York State, I never cease to be awestruck by the beauty of our changing seasons, and cannot imagine living in a place where the years pass with scant visible change in the environment. Yet there is one season I cannot abide, and it has arrived with a vengeance—hunting season.
Mind you, I have no problem with safety-trained folks, traipsing through the woods this time of year, toting rifles or compound bows. What I object to are all the unlicensed, eight-legged hunters which have (literally) come out of the woodwork lately: ticks. A decade ago it was unusual to find a single tick after a northern NY wilderness weekend, but now in many places all you have to do is set foot in the brush and you’re ambushed by hordes of black-legged ticks, commonly known as deer ticks.
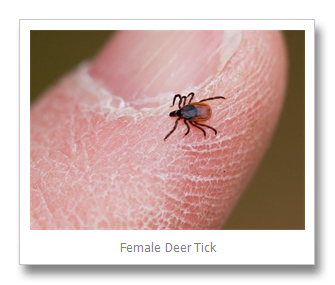
Smaller and more difficult to see than most other ticks, deer ticks can transmit a number of serious diseases, including Lyme, Babesiosis, Anaplasmosis, and Powassan virus. In fact, it’s possible for two or more diseases to be transferred by a single tick bite. A high percentage of infections come from the immature or “nymph” stage deer tick, tinier than a poppy seed and nearly impossible to detect, (at least for those of us over fifty) without magnification. The adults are not exactly huge, being a bit smaller than a sesame seed, but they are the ones most active during hunting season, and any time when winter temperatures get above freezing.
In light of new research, revealed this summer, we need to update our understanding of the risks posed by deer ticks. Honestly, not even Captain Hook is more terrified of ticks than I am, but no one can afford to stick their head in the sand. We’d probably end up with grit in our ears, which is uncomfortable, and worse yet, we could contract a tick-borne disease.
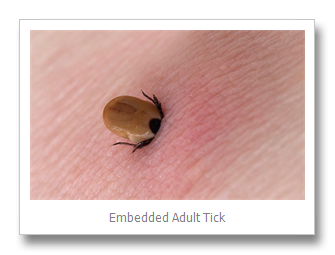
In a July 2016 presentation to fellow physicians, Dr. Nevena Zubcevik of the Harvard Medical School, and co-director of the Dean Center for Tick-Borne Illnesses, warned that the medical community is not keeping up with current findings. For example, “The conception that the tick has to be attached for 48 hours is completely outdated,” she said, citing studies that show ticks can transmit disease in as little as 10 minutes.
She also stated that the 2-day course of Doxycycline currently prescribed when an embedded tick is discovered is worthless, saying “It should be a 20-day thing [...] regardless of time of [tick] engorgement.” Equally surprising is the fact that only 20% of Lyme cases show the classic “bull’s-eye rash,” or Erythema Migrans. In the past, it was believed that the majority of Lyme cases exhibited this outward-spreading rash.
But what may be the most troubling recent finding is the idea that Lyme tests are spectacularly unreliable. Zubcevik points out that there are at least 10 different variants of Borrelia burgdorferi, the organism responsible for Lyme, most of which do not show up on the ELISA or Western blot tests. And if that wasn’t bad enough, a newly-identified, closely-related species of pathogen, Borrelia miyamotoi, also causes Lyme, and does not show up on any tests at all. Dr. Zubcevik contends that under current testing guidelines, 69 of 100 Lyme cases will not be diagnosed in a timely fashion.
In a good-news, bad-news finding, it appears that some cases of so-called “early-onset dementia,” and even certain mental illness diagnoses, may be caused by Lyme, but that they can potentially be reversed through treatment. Singer and songwriter Kris Kristofferson’s dementia was completely cured after he was properly diagnosed with Lyme and treated. “Sudden-onset dementia should be a red flag for Lyme,” says Dr. Zubcevic.
Although prompt treatment cures Lyme,, in the majority of infected people, it’s not always as simple as taking pills and feeling improvement. Lyme symptoms can persist for weeks, or months, after the standard 3-week treatment has ended. In rare cases it can be a year or more. This is called “Post-Treatment Lyme Disease Syndrome,” and its causes are not well understood.
How likely is it that “your” tick will be infected with Lyme? A 2014 NYS Department of Health study, carried out in conjunction with Paul Smith’s College, found that the rate of Lyme-infected ticks, in northern NYS, ranged between just over 50% (St. Lawrence County) to nearly 80% (Clinton County). I do not gamble, but am pretty sure those are not good odds.
To avoid being bitten by ticks, people who work or play outdoors need to take precautions that weren’t necessary in the past. Avoiding ticks is the first order of business. Ticks “quest” at the tips of tall grass or brush, waiting to cling to the next warm body that brushes against them. The Centers for Disease Control and Prevention (CDC) recommend using products containing 20-30% DEET on exposed skin. (Unfortunately, research indicates herbal repellants range in effectiveness between 0% to about 30% as compared to DEET.) Clothing, footwear and gear such as tents can be treated with products containing the active ingredient Permethrin. Hikers should stick to marked trails.
Homeowners can clear brush, weeds and tall grasses from the edges of their yards. Ticks like to hide out under leaf litter (which is why sprays are not effective against them), so maintaining a yard perimeter that’s raked clean can help discourage ticks. Pets should be treated regularly, with an anti-tick product, so they don’t bring deer ticks into the home. Talk to your vet about getting your pets vaccinated against Lyme (sadly there is no human vaccine at the moment).
Despite their name, deer ticks feed on—and infect—many wild critters, particularly our native and ubiquitous white-footed mouse. Because of ticks’ prevalence, people who spend a lot of time outside will eventually have contact with deer ticks. This is where tick hygiene comes in.
Shower and wash thoroughly every evening and then check for ticks. They like hard-to-see places such as the armpits, groin, scalp and the backs of the knees, so look closely in these areas. If you find a tick has latched onto you, the CDC recommends you remove it by grasping it as close to the skin as possible with tweezers and pulling straight up until it releases. You may have to pull hard if it has been feeding for some time. Don’t twist it or use heat, petroleum jelly or other home remedies to get it to release, as this can increase the chances of disease transmission.
Conventional wisdom was that “typical” early symptoms of Lyme disease included severe headaches, chills, fever, extreme fatigue, joint pain and dizziness. With further research, it is evident that early symptoms can vary drastically, making Lyme all the harder to diagnose. Irritability, mood changes, mental confusion, heart palpitations and forgetfulness may be the first manifestations of Lyme. These early signs may go away on their own, but the Lyme organism will cause even more serious health issues in the future if ignored.
If you’ve been bitten by a tick and have any of these symptoms, see your doctor right away. She or he can order a blood test, or may even prescribe antibiotics based on symptoms. For more information, go to the CDC website at http://www.cdc.gov/lyme or to the NIH site at https://www.niaid.nih.gov/topics/lymeDisease.
Follow tick-hygiene guidelines so you don’t fall prey to ticks this autumn. Hunting should be a choice.
By Paul Hetzler
Paul Hetzler is a Horticulture and Natural Resources Educator at Cornell Cooperative Extension, in Canton, NY. He writes a series of humorous and informative essays for a number of newspapers and journals. Subjects range from trees, gardens, insects, native plants, water, wildlife and other natural resources topics.